What are indicators?
Indicators are succinct summaries of, sometimes sophisticated, data collection and analysis. Their simplicity is effective. Indicators can stimulate a member of the public to organize for change, a patient to insist on her rights, a researcher to initiate a study, a programme manager to review an intervention, a donor to prioritize differently, or a policymaker to re-allocate funds. Indicator simplicity can also mislead.
Indicators summarise observations made at some place and some time and always include some uncertainty or error, whether statistical or human. When combined, several indicators show a pattern in a jigsaw but cannot complete the picture; at best they stimulate further investigation and action.
Proliferating health indicators
Practitioners have long used indicators to describe issues of public health concern and to assess progress in handling them. But the advent of computers has made it possible to measure any number of them. Over the last half decade numerous global declarations and programmes have committed to meeting indicators with specified targets.
- In 1978, the Declaration of Alma Ata which outlined a global strategy to attain Health For All. To measure attainment of this goal, the WHO proposed 12 indicators for countries to report internationally and a choice of 19 plus indicators for national use, classified as: health policy, social and economic, provision of health care and health status.
- In 1990, the World Summit for Children laid out 33 goals (some with multiple indicators) to achieve by the year 2000.(14) During the 1990s, WHO identified 15 indicators to describe reproductive health.
- Other programmes developed lists of indicators, for example, in 1994, the HIV/AIDS programme began with ten preventive indicators and by 2014, WHO/UNICEF and UNAIDS were collecting 78 indicators reflecting preventive, promotive, curative and rehabilitative interventions.
- In 2014, the Global Fund used 114 indicators to monitor just three diseases: AIDS, tuberculosis and malaria.
- The Millennium Declaration laid out eight goals – of which four related directly to health – with 21 targets and 60 indicators.
- The Sustainable Development Goals (SDGs) committed to achieving 17 goals, 169 targets and 232 indicators by 2030 – of which 13 targets and 26 indicators are directly related to health, including the target of Universal Health Coverage (UHC).
In 2014, WHO and partners made a conservative estimate that some countries regularly reported as many as 600 indicators to donor partners and international disease programmes or to comply with international resolutions; often with different definitions and reporting frequencies. To reduce and rationalise national data collection, WHO led an interagency working group which created The Global Reference List of 100 Core Health Indicators.
Leaving no-one behind
Disaggregating indicators
In 2008, the WHO Commission on the Social Determinants of Health drew attention to widespread and persistent challenge of health inequalities – systematic differences in the health status of a jurisdiction’s sub-populations. These become apparent when investigators disaggregate indicators by attributes such as: socio-economic status (usually obtained from survey data on individual/household income/wealth/education); racial or ethnic group (also typically from surveys or, in more developed settings, census data); and geographic location (e.g. rural versus small urban, versus large urban).
The SDGs explicitly address equity in their vision of ‘no-one left behind’. To measure progress towards this vision, analysts must disaggregate SDG indicators at least by residence, wealth, education, sex, and age. Disaggregating indicators in this way places an even higher burden of data collection and analysis on country reporting systems.
Universal Health Coverage
SDG target 3.8 – to achieve UHC, including financial risk protection – is fundamental to meeting all health-related SDG targets and offers particular challenges for indicator measurement. Indicators of coverage and financial protection summarise sub-indicators which require data that are not readily available or of high quality in many countries.
Indicator 3.8.1, ‘coverage of essential health services’, comprises several proxy indicators that are not direct measures of health service coverage because most countries lack suitable data. Proxy indicators such as density of physicians and hospital beds and use of services, offer imprecise impressions of service coverage and are difficult to interpret without knowledge of their optimal levels.
- The SDG indicator of effective service coverage is ‘the proportion of people in need of services who receive services of sufficient quality to obtain potential health gains’ whereas an indicator of service coverage, is ‘the proportion of people in need of a service that receive it, regardless of quality’.
- The SDG indicator for financial protection is ‘the proportion of the population with large household expenditures on health as a share of total household expenditure or income’. The indicator classifies out-of-pocket expenditures on health as catastrophic when they exceed a 10 per cent or a 25 per cent threshold of total household expenditure or income.
Indicators for programme management
Frameworks
Conceptual frameworks provide a logic to select and interpret indicators and explain more of reality. They can be, for example, mathematical models that explain associations between health outcomes and their determinants; logical frameworks to monitor health sector performance; or depictions of theories of change.
The Global Reference List uses two frameworks to classify its 100 indicators:
- First the list classifies indicators by four health domains (with sub-domains), that is: health status (mortality by age and sex, mortality by cause, morbidity and fertility); risk factors (nutrition, infections, environmental risk factors, non-communicable disease risk factors, and injuries); service coverage (reproductive, maternal, newborn, child and adolescent, immunization, HIV, HIV/TB, tuberculosis, malaria, neglected tropical diseases, screening and preventive care, and mental health) and health systems (quality and safety of care, access, health workforce, health information, health financing, and health security).
- Secondly, the list classifies indicators as inputs, processes, outputs, outcomes and impact, using the International Health Partnership (IHP+) Common Monitoring and Evaluation Framework
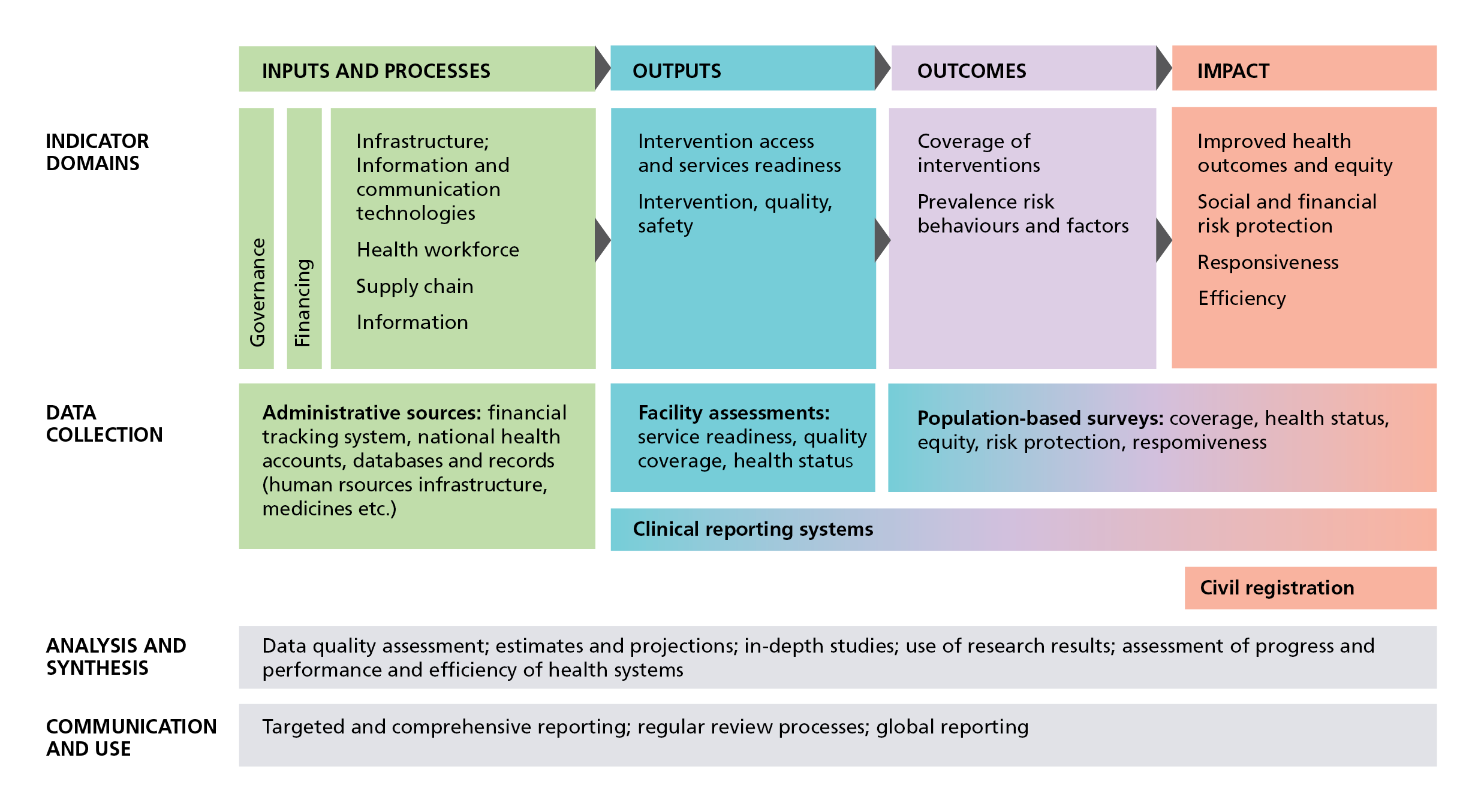
International Health Partnership (IHP+) Common Monitoring and Evaluation Framework
IHP+ developed this results-chain framework to assist countries to assess the performance of their national health strategies, and so it links national and global reporting systems. The IHP+ Framework also identifies the data sources countries can use to measure these core indicators. The framework facilitates temporal and cross-country comparisons but using the same set of indicators everywhere to track complex interventions risks losing sight of different patterns of causality of mortality and ill-health in diverse settings.
Selecting indicators
While epidemiologists select indicators to meet their research questions, programme managers identify indicators to describe inputs, outputs, outcomes and impacts within their chosen framework. Technical considerations in selecting indicators include:
- Clarity about the population and timescale to which indicators refer.
- Reporting frequency.
- Whether data sources are available and reliable.
- Whether is possible to disaggregate indicators at multiple levels (national, state, local, and community) and for selected populations.
Programme managers increasingly involve stakeholders in choosing indicators. This enhances the relevance of the indicators and the possibility that the general public and health communities understand the results.
Indicators should: 1) reflect significant national health topics seen as having some social value; 2) be underpinned by government health objectives; and 3) address problems that public policy and operational initiatives could improve.
Managers should choose and define indicators consistently across programmes, where possible selecting from the Global Reference List.
Once an issue becomes a policy priority, managers must develop methods to monitor implementation over time. Especially during the initial phase of a disease-specific programme, indicators may change. Desirable indicators may not be immediately measurable, and what can be measured may not be the most relevant statistic for programme planning. Indicator selection should be sufficiently flexible to embrace new measurement methods with regularly updated measurement strategies.
Indicators require target and baseline values against which their achievement can be measured or benchmarked. Targets may be absolute or relative – achievement of a defined percentage change compared with baseline.
Where appropriate, targets will be in line with those for the SDGs.
- Absolute global targets make achievement harder for countries with baselines furthest from the target.
- Relative targets are easier to achieve for all countries but their use risks further exacerbating inequities between countries.
Challenges
Health indicators provide limited, but often useful information, about the state of a population’s health and the functioning of its health system. Indicators cannot describe all aspects of health programmes. They offer insights by facilitating comparisons over time and within and between countries and populations.
Indicators are indirect statements or measures of something more complicated. Nonetheless, because they frequently measure progress towards targets, indicators tend to drive programmes and influence donor funding decisions. By rewarding target attainment with additional funds , for example, through performance-based funding mechanisms, the international development system exerts pressure to move indicators in the right direction.
Once the management team has adopted an indicator, programme interventions tend to focus on improving that indicator rather than on addressing the intended impact. For example, if managers use skilled attendance at delivery as a proxy for maternal mortality, they will try to ensure women deliver in the presence of a skilled attendant. But levels of maternal mortality may be high because of other factors, such as unsafe abortions or elevated levels of malaria.
It is easier to guide programmes using readily quantifiable indicators such as numbers of vaccines distributed instead of exploring motivating factors that might contribute to successfully distributing the vaccines. Qualitative information, on the other hand, can explain the context in which the programme functions and how participants perceive its activities.
Ultimately, indicator reliability and validity depend on the quality of country information systems that provide data for their calculation; the quality of these systems is, in turn, threatened by the burden of indicators they measure.
Contents
Source chapter
The complete chapter on which we based this page:
Additional resources
Karpati A., Ellis J. (2019) Measure, Inform, Build: Enabling Data-Driven Government Policymaking. In: Macfarlane S., AbouZahr C. (eds) The Palgrave Handbook of Global Health Data Methods for Policy and Practice. Palgrave Macmillan, London.
The World Health Organization Coronavirus disease (COVID-2019) situation reports are based on data provided to them by national governments.
WHO also provides additional information including a dashboard on this website.
WHO has developed a global reference list of 100 core health indicators and provides annual updates. The 2018 version of the core indicators also describes all the health-related SDG indicators adding those that are not included in the core 100.
The WHO Global Health Observatory provides summaries of indicators and access to data on 30 health themes.
The United Nations Statistics Division maintains values of all the MDG and SDG indicators by country.

